Contact:
Dutch Ministry of Health
Dutch Nursing Specialist Register
Dutch Professional Nurse Practitioner Organization
Role
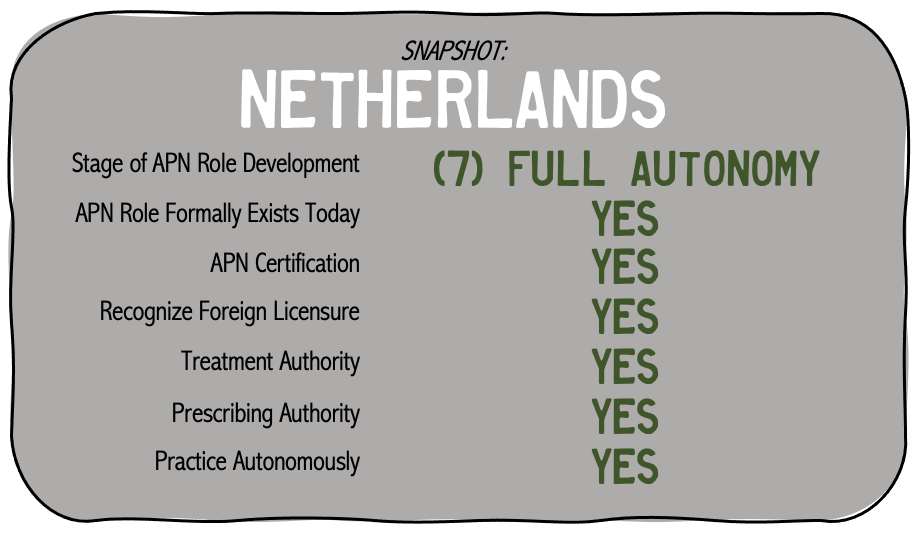
The role of Advanced Practice Nurses in the Netherlands is the Nurse Practitioner or “Verpleegkundig (VSR, 2022). Introduction of this role started in 1997 (Storedur & Leonard, 2010; Van den Brink et al., 2019). The Clinical Nurse Specialist role in the Netherlands had initially developed as an alternative health provider for general practice physicians based on a general practitioner shortage (Dierick-van Daele, 2010; Stordeur & Leonard, 2010; Zwijnenberg & Bours 2012). Progressively, the role expanded as the health system responded with generalized acceptance and improvement of cost efficiency and outcomes (Maier, 2019; Van den Brink, 2019; VSR, 2019). The scope of practice for Dutch Nurse Practitioners primarily includes:
- Advanced assessment (Dierick-van Daele, 2010)
- Diagnosing and making decisions for further treatment (Dierick-van Daele, 2010)
- Full Prescriptive authority within specialization (Maier, 2019)
- Provision of procedures necessary for medication treatment (Zwinjenberg & Bours, 2012)
- Referrals to primary or secondary services (Dierick-van Daele, 2010)
- Autonomous practice without physician supervision (Van den Brink et al., 2019)
As the role has progressively developed, Van den Brink et al. (2019) identified the practice of care in hospital settings and identified
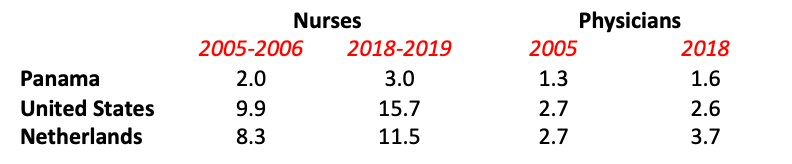
Since the introduction of the Nurse Practitioner role in the Netherlands, studies began showing that the role significantly addressed areas of patient care that were not previously adequately addressed by their physician staff (Stordeur & Leonard, 2010). While the role is not intended to replace that of physicians, it has been greatly observed as a complimentary role and is pursuing more autonomous roles for Nurse Practitioners to perform patient care in patients homes and management of chronic illnesses (Storeur & Leonard, 2010; Maier, 2019).
Education and Certification
A four-year bachelor degree is necessary to work as a registered nurse in the Netherlands (Robinson & Griffiths, 2007). The advancement of nursing practice to become a Certified Nurse Specialist requires an individual to receive a 2-year dual Master of Advanced Nursing Practice (MANP) degree (Dierick-van Daele, 2010; Stordeur & Leonard, 2010; VSR 2022). In the event an advanced practice nurse would like to practice in the Netherlands, there are several nations of the EU including Switzerland, Iceland, Norway, or Lichtensetin in which registration is transferrable (VSR, 2022). If an individual received their APN training outside of these nations, they will need to first complete the MANP degree, however individuals may qualify for a shortened trajectory based on their previous training (VSR, 2022).
The Dutch have been very proactive in developing a model to facilitate this role development, including having their APN students experience through immersion the Nurse Practitioner role outside their country (Ter Maten & Garcia-Maas, 2010). Registration for Advanced Practice Nurses in the Netherlands requires individuals to register under a separate registry (the Verpleegugkundig Specialist Register [VSR]) from that of registered nurses, maintained by a division of the Central Information Centre for Professional Practitioners, an branch under the Ministry of Health, Welfare, and Sport (Robinson & Griffiths, 2007; VSR, 2017).
Specialties
Based on the needs of the Dutch health system, there two main specializations: general (or somatic) health and mental health as follows (VSR, 2017). A link to the Professional Competency Framework can be found here.
The curriculum for further specialization (i.e. cardiology, primary care) is then incorporated within the specific graduate coursework of one of the above specialties (VSR, 2017).
Have information to add to this page?
References:
Delamaire, M. & Lafortune, G. (2010). Nurses in advanced roles: A description and evaluation of experiences in 12 developed countries. OECD Health Working Papers, 54, OECD Publishing.http://dx.doi.org/10.1787/5kmbrcfms5g7-en
Dierick-van Daele, A. (2010). The Introduction of the Nurse Practitioner in General Practice [electronic publication]. Schering-Plough. Retrieved from: http://arno.unimaas.nl/show.cgi?fid=20140
Maier, M.B. (2019). Nurse prescribing of medicines in 13 European countries. Human Resources for Health. 95(2019), doi:10.1186/s12960-019-0429-6
Pulcini, J., Jelic, M., Gul, R, Loke, A.Y. (2009). An international survey on advanced practice nursing, education, practice, and regulation. Journal of Nursing Scholarship, 42(1),31-39. doi: 10.1111/j.1547-5069.2009.01322.x
Robinson, S. & Griffiths, P. (2007). Nursing education and regulation: International profiles and perspectives [online publication]. Retrieved from:http://eprints.soton.ac.uk/348772/1/NurseEduProfiles.pdf
Sheer, B. & Wong, F.K. (2008). The development of advanced nursing practice globally. Journal of Nursing Scholarship, 40(3),204-211.
Stordeur, S. & Leonard, C. (2010). Challenges in physician supply planning: The case of Belgium. Human Resources for Health, 8(28),1-11. doi:10.1186/1478-4491-8-28
Ter Maten, A. & Garcia-Maas, L. (2010). Dutch advanced nursing practice students: Role development through international short-term immersion. Journal of Nursing Education, 48(4), 226-231.
Van den Brink, G.T.W.J., Kouwen, A.J., Hooker, R.S., Vermeulen, H. & Laurant, M.G.H. (2019). An activity analysis of Dutch hospital-based physician assistants and nurse practitioners. Human Resources for Health. 78(2019). doi:10.1186/s12960-019-0423-z
Verpleegkundig Specialisten Register [VSR] (2017). More information (in English) about the profession of the certified nurse specialist: The nurse practitioner in the Netherlands. Retrieved from: https://www.venvn.nl/media/zvofiilk/additional-information-about-the-certified-nurse-specialist.pdf
Verpleegkundig Specialist Register [VSR] (2022). Foreign graduates: The nurse practitioner in the Netherlands [webpage]. Retrieved June 28, 2022 from: https://www-venvn-nl.translate.goog/registers/verpleegkundig-specialisten-register/registratie/buitenslands-gediplomeerden/?_x_tr_sl=auto&_x_tr_tl=en&_x_tr_hl=en&_x_tr_pto=wapp
Zwijnenberg, N.C. & Bours, G.J. (2012). Nurse practitioners and physician assistants in Dutch hospitals: their role, extent of substitution and facilitators and barriers experienced in the reallocation of tasks. Journal of Advanced Nursing, 68(6),1235-1246. doi: 10.1111/j.1365-2648.2011.05823.x
[Initially published 16 Aug 2013; revised 1 Jul 2022, revised 9 Jun 2024]