Contact:
Jamaican Association of Nurse Anesthetists (JANA)
Jamaica Association of Nurse Practitioners (Facebook Page)
Jamaica Ministry of Health
Nursing Council of Jamaica
University of West Indies, School of Nursing
Role
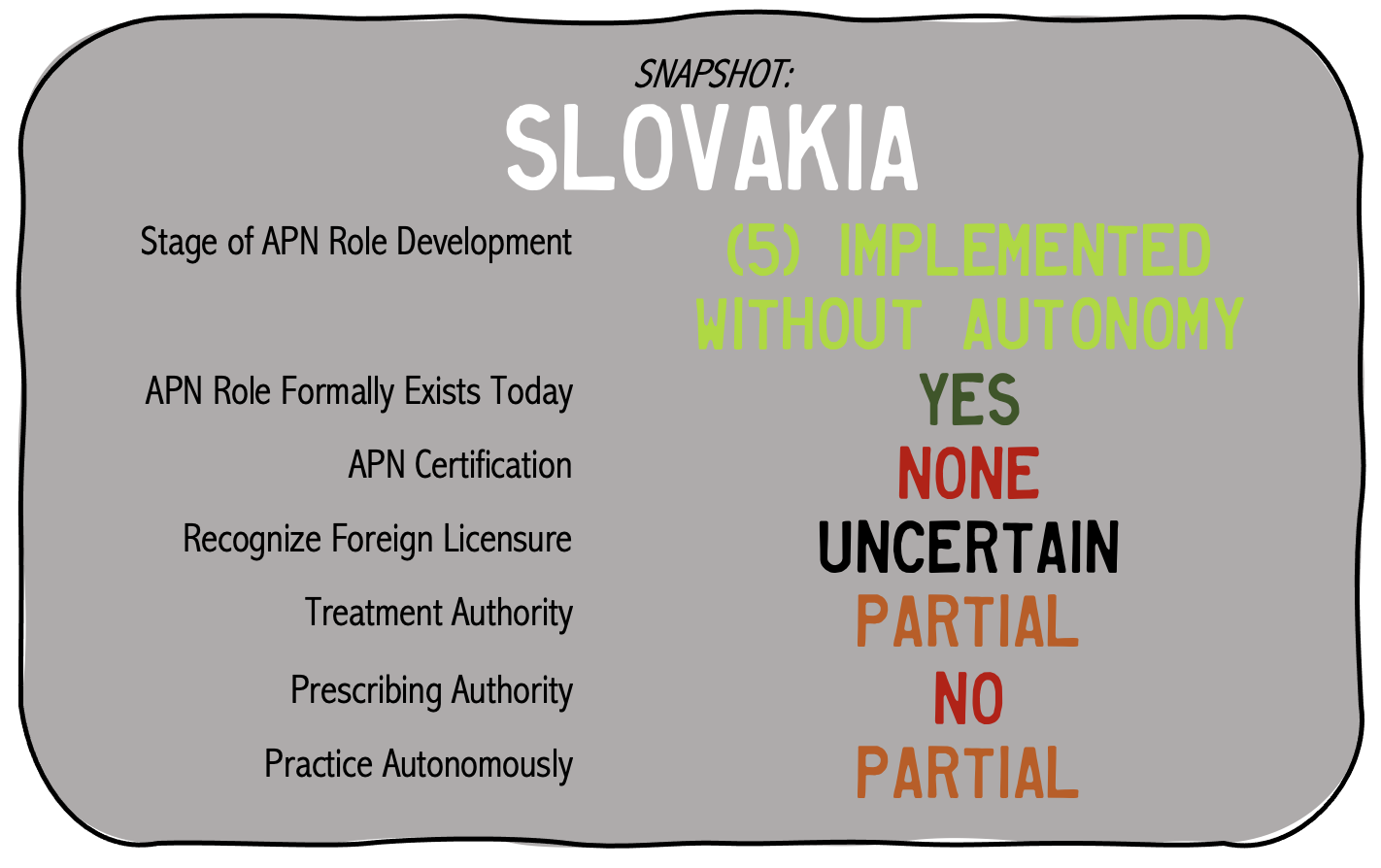
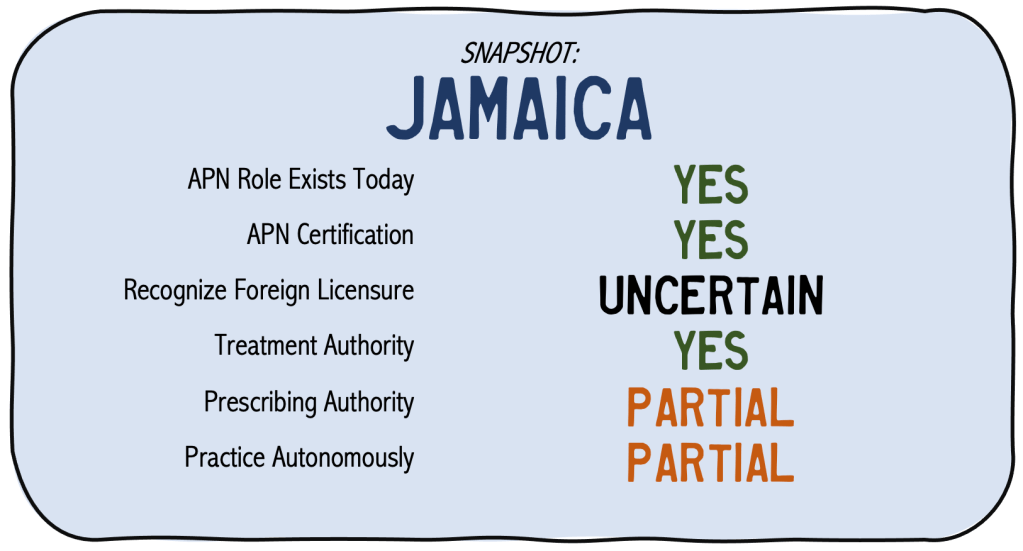
The role of the Advanced Practice Nurse (APN) was introduced in Jamaica in the 1970s largely driven by the lack of physicians in the country (NP / APN Network, 2022, p. 5, Zug et al, 2016). There are two main roles, identified as a Family Nurse Practitioner and Nurse Anesthetist.
Nurse Practitioner (NP)
The Nurse Practitioner role revolves around providing primary care services to patients, particularly in underserved and rural areas (Henry, 2019; Zug et al, 2016). More specifically, a Nurse Practitioner in Jamaica performs the following duties (Henry, 2019):
- Assess patient needs
- Interpret diagnostic and laboratory tests
- Diagnose illness and disease
- Prescribe medication
- Formulate treatment plans
At this time the role is still regarded as in development to “update and increase the scope of APN practice ” as Nurse Practitioners are not able to independently prescribe medication without oversight by a physician (Henry, 2019; NP / APN Network, 2022, pg. 5; Zug et al, 2016).
Nurse Anesthetist (CRNA)
Also identified largely as the Certified Registered Nurse Anesthetist (CRNA), the role was largely developed in the 1980s to mitigate the anesthesia needs and costs throughout the country as only 40 anesthesiologists were in the country in 2015 and the country at the same time supported the anesthesia needs by having 50 CNRAs (IFNA, 2015).
Education and Certification
As of 2002, education required for practice as a Nurse Practitioner was increased to a master’s level program through the West Indies School of Nursing (Zug et al, 2016). Once completing the educational requirement, the APN obtains certification to practice in the country which is regulated by the Nursing Council of Jamaica (NP / APN Network, 2017). The program at the University of the West Indies (UWI) requires at least 5 years of nursing experience while not attending an educational institution and licensure from any of the 16 countries that the UWI serves (including Bahamas, Barbados, Belize, the British Virgin Islands, Cayman Islands, Dominica, Granada, Jamaica, Montserrat, St. Kitts and Nevis, St. Lucia, St. Vincent, the Grenadines, Trinidad and Tobago and Turks and Caicos (UWI, 2022).
For the role of the Nurse Anesthetist, a master’s level degree has been required since 2007, and educational requirements include a 32 month program that does involve a 6 month internship through the UWI (IFNA, 2015). Biennial re-licensure is required by the Nursing Council of Jamaica (IFNA, 2015).
Specialties
The two main roles of the APN in Jamaica are:
- Nurse Practitioner
- Nurse Anesthetist
Have information to update this page?
References:
Henry, O. (2019). Legislative framework for NPs to practice far advanced. Jamaica Information Service. Retrieved May 16, 2022 from: https://jis.gov.jm/legislative-framework-for-nps-to-practise-far-advanced/
International Federation of Nurse Anesthetists [INFA] (2015). Jamaica. Retrieved May 16, 2022 from: https://ifna.site/country/jamaica/
NP / APN Network (2017). Country specific practice profiles. Retrieved May 16, 2022 from: https://international.aanp.org/Practice/Profiles
NP / APN Network (2022). INP/APN Network Bulletin. 33rd Issue. Geneva. Retrieved from: https://international.aanp.org/Content/Bulletins/May2022.pdf
University of West Indies [UWI] (2022). The UWI School of Nursing. Retrieved May 16, 2022 from: https://www.mona.uwi.edu/nursing/content/family-nurse-practitioner
Zug, et al. (2016). Advanced practice nursing in Latin America and the Caribbean: Regulation, education and practice. Revista Latino-Americana de Enfermagem. 24(e2807):1-9. doi:10.1590/1518-8345.1615.2807